Arthritis and total knee replacement
Arthritis is a disease which causes the cartilage in a joint to gradually degrade, resulting in pain and stiffness which can gradually become debilitating. Around 15% of Australians currently suffer from it in some capacity.
The most common type of arthritis is osteoarthritis. Also known as degenerative or ‘wear-and-tear’ arthritis, it most commonly affects the knee joint. It generally worsens over time and cannot be cured, although timely intervention can delay progression and effectively manage symptoms.

Symptoms & treatment
Primary knee arthritis symptoms include pain, swelling, and joint stiffness. Pain may worsen when on movement or following periods of immobility, such as standing after sitting for a while or after getting out of bed in the morning.
This is often accompanied by ‘crunching’ sounds or sensations in the joint during movement, as well as a decreased range of motion.
Treatment for knee arthritis
The initial stages of arthritis in the knee are treated conservatively. Techniques such as activity management and anti-inflammatory medications can help manage arthritis pain in the knee. Your doctor may recommend a walking aid – such as a cane or crutches – to improve your mobility.
Surgery may be considered if symptoms cannot be managed effectively. The typical recommendation is knee joint replacement, which involves removing the diseased bone and replacing it with a prosthetic.
Total knee replacement surgery
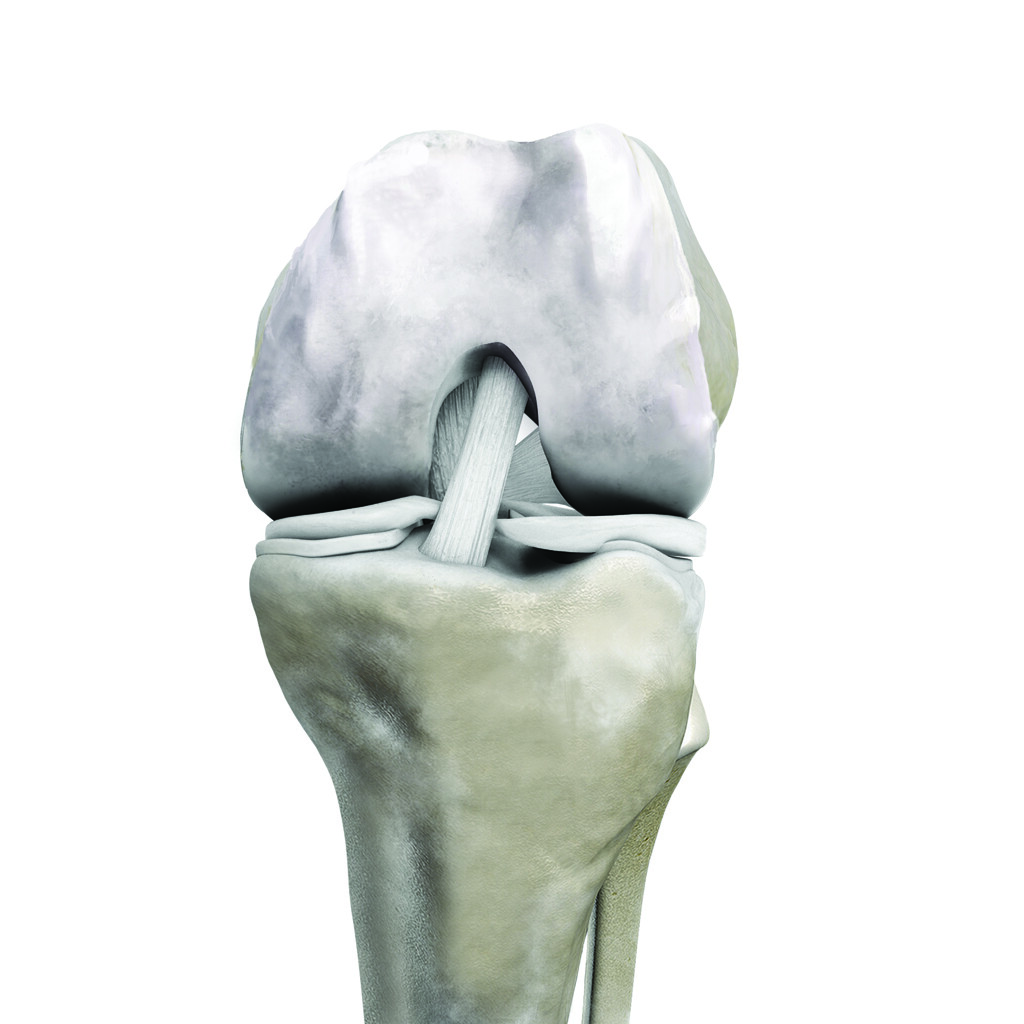
Total knee replacement is used to treat arthritis which does not respond to conservative management and which is not localised to one area of the knee.
It involves cutting away the diseased sections of both bones in the knee and implanting a prosthetic replica.
Where arthritis is localised to one area of the knee, a unicompartmental (partial) knee replacement can often be performed. This is a less extensive surgery which replaces only one compartment.
Indications for total knee replacement
Ulceration of the skin around the knee or leg may impact your suitability as it greatly increases the risk of post-surgical infection. Very weak knee and thigh muscles may not provide sufficient support for the prosthetic and make replacement not viable.
The shape of the bone, extent of damage, and type of arthritis can also impact suitability. Dr Jonathan Cabot, orthopaedic surgeon in Adelaide, will assess your suitability for surgery and determine the ideal approach as part of your pre-surgical consultation.



Recovering from total knee replacement
Are you experiencing severe arthritis and feel you may need a total knee replacement in Adelaide?
Contact Dr Jonathan Cabot at (08) 8267 8228 and schedule a consultation with a highly experienced orthopaedic knee surgeon.
Frequently Asked Questions
Common knee arthritis symptoms include:
- Persistent pain in the knee, especially after activity or during movement
- Stiffness in the knee joint, particularly after periods of inactivity, such as sitting or sleeping
- Swelling around the knee joint due to inflammation or excess fluid
- Difficulty in fully bending or straightening the knee
- A sensation of grinding or catching when moving the knee, often due to the loss of cartilage
- In advanced cases, the knee may appear deformed or misaligned
Knee arthritis is diagnosed through:
- Medical History: Dr Cabot will review the patient’s medical history, symptoms, and any previous injuries.
- Physical Examination: A thorough examination of the knee to assess pain, range of motion, and swelling.
- Imaging: X-rays, MRIs, or CT scans are often used to visualise the extent of joint damage and cartilage loss.
- Laboratory Tests: Blood tests may be conducted to rule out other conditions like rheumatoid arthritis.
Knee arthritis is treated with:
- Medications: Pain relievers, anti-inflammatory drugs, and corticosteroid injections can help manage symptoms.
- Physical Therapy: Exercises to strengthen the muscles around the knee and improve flexibility.
- Lifestyle Modifications: Weight management and low-impact activities can reduce strain on the knee.
- Assistive Devices: Braces or shoe inserts can help support the knee and alleviate pain.
- Surgery: In advanced cases, surgical options like arthroscopy, osteotomy, or knee replacement may be considered.
Knee replacement surgery is recommended for arthritis when:
- Pain persists despite conservative treatments and significantly affects daily activities or sleep.
- Imaging shows extensive damage to the cartilage or bone, leading to joint instability or deformity.
- The patient’s ability to move the knee is severely restricted, and mobility aids are needed.
- Non-surgical treatments such as medications, physical therapy, and injections have not provided adequate relief.
- The arthritis severely impacts the patient’s quality of life, and other treatment options are no longer effective.
Differences between partial and total knee replacement include:
- Total Knee Replacement: The entire knee joint is replaced with artificial components, including the femur (thigh bone), tibia (shin bone), and sometimes the patellar (kneecap). This is typically recommended when arthritis affects the entire knee.
- Partial Knee Replacement: Only the damaged portion of the knee is replaced, preserving the healthy bone and cartilage in the rest of the knee. This option is suitable for patients with arthritis confined to one part of the knee.
Factors that determine the best candidates for total knee replacement surgery include:
- Severity of Arthritis: Advanced arthritis with significant joint damage.
- Age: While total knee replacement is commonly performed in older adults, younger patients with severe arthritis may also be candidates.
- Overall Health: Patients should be in goo general health to undergo surgery, as conditions like heart disease or uncontrolled diabetes can increase risks.
- Weight: Obesity can affect both the outcome of surgery and the lifespan of the implant, so weight management is often considered.
- Activity Level: Total knee replacement is recommended for patients with lower activity levels, as high-impact activities can wear down the implant over time.
Total knee replacement recovery typically takes several months. Most patients stay in the hospital initially for 2-3 days after surgery. The first 6 weeks involve wound healing, pain management, and the start of physical therapy to regain mobility and strength. By 3 months, many patients experience significant improvements in pain function, though stiffness and swelling may persist. It can take up to 6 months to a year to fully recover, with continued improvement in strength, flexibility, and function. Regular follow-ups and adherence to a rehabilitation program are crucial for optimal recovery.
Are you experiencing severe arthritis and feel you may need a total knee replacement in Adelaide?
Contact Dr Jonathan Cabot at (08) 8267 8228 and schedule a consultation with a highly experienced orthopaedic knee surgeon.